CASE HISTORY
59-Year-old lady, a known case of chronic liver disease with portal hypertension presented with progressive left hemiparesis over three months. There was no history of fever/ weight loss/previous head injury.
Plain CT Brain and CE-MRI Brain were done to evaluate the same.
Investigations
LFT: Bilirubin total – 1.3mg/dl, bilirubin direct – 0.7mg/dl, SGOT -102U/L, SGPT – 68U/L, ALP – 185U/L, Serum albumin – 4.8g/dl, serum globulin – 4.8g/dl, albumin: globulin – 0.46, PT- 17.3s, APTT- 36.6s (Deranged).
CRP- 19mg/L (raised), PLC and RBC counts are reduced, TLC – 5560/cu.mm (within normal limits).
CASE CONTRIBUTED BY
Dr. Namitha Ajith Kumar, Department of Radiology, Manipal Hosipitals, Kanakapura Road, Bangalore.
Dr. Anusha shree Thaneeru, Department of Radiology, Manipal Hosipitals, Kanakapura Road, Bangalore.
Dr. Chirag G, Department of Radiology, Manipal Hosipitals, Kanakapura Road, Bangalore.
Dr. Chaitra P. Adiga, Consultant Radiologist, Manipal Hosipitals, Kanakapura Road, Bangalore.
Dr. Yashwanth A S, Consultant Radiologist, Manipal Hosipitals, Kanakapura Road, Bangalore.
Dr. Lakshmikanth G N, Consultant Radiologist, Manipal Hosipitals, Kanakapura Road, Bangalore.
Dr. Veekshit Shetty, Consultant Neurosurgery, Manipal Hosipitals, Kanakapura Road, Bangalore.
Dr. Arati Kamble, Consultant Microbiologist, Manipal Hosipitals, Kanakapura Road, Bangalore.
DESCRIPTION
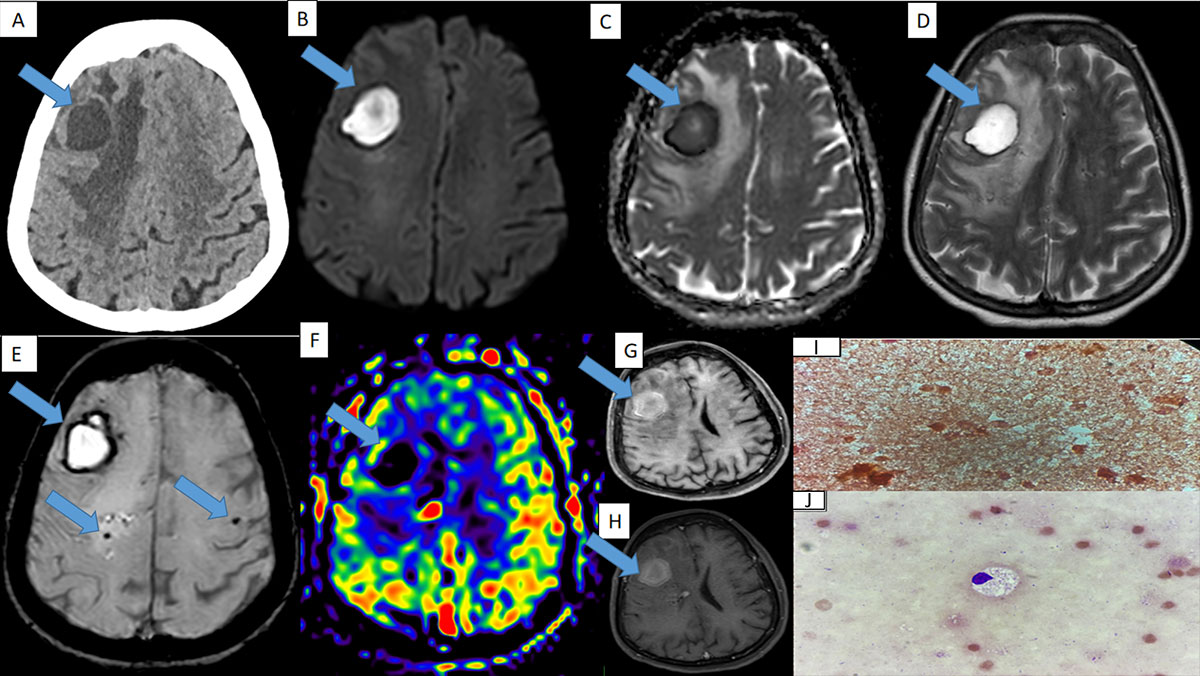
- A :Axial section of plain CT brain shows a well defined hypodense lesion in the right middle frontal gyrus with extensive perilesional edema in the right frontal lobe white matter.
- Band C : The lesion shows central diffusion restriction.
- D: Axial T2 sequence shows a well defined T2 hyperintense lesion seen in the right middle frontal gyrus with peripheral hypointense rim and extensive perilesional edema.
- E: Axial section of susceptibility weighted sequence shows peripheral blooming around the lesion with few microbleeds adjacent to the lesion.
- F: Axial section of arterial spin labelling sequence shows no perfusion at the centre and periphery.
- G and H: Axial section of pre-contrast T1 FS sequence and post-contrast T1 sequence showing peripheral enhancement on post contrast study.
- I: Gram stain – No pus cells. No organisms seen.
- J: Sediment smears from the fluid sample showed macrophages on a background of RBCs on Leishman stain. Pus culture report from specimen obtained from the showed no growth after 48hours of incubation.
Diagnosis: Chronic Encapsulated Intracerebral Hematoma (CEIH)
Discussion:
- CEIH is a extremely rare form of intracerebral haemorrhage with progressive Clinicoradiological features and is often misdiagnosed as abscess or tumors1.
- Intracerebral hematomas usually resolve spontaneously. Rarely, they become encapsulated and enlarge from repeated internal bleeding after a delay2. This expansion can cause neurological deficits and features of raised intracranial pressure.
- Patients may also have progressive neurological deficits, such as weakness, visual deficit, behavioural changes, or dysphasia. Acute presentation with seizure can also occur.
- Associations of CEIH include, vascular malformations, coagulation disorders, post radiosurgery/ radiotherapy, post traumatic or spontaneous parenchymal hemorrhage and neoplasms3.
- It can occur in any age group, with a mean age of 44 years and has been reported to occur in the cortical or subcortical area3.
- Generally, the time course of CEICH is not strictly defined, however, CEICH is reported to occur between 2 and 4 weeks after onset of ICH3.
- CEIH is characterized by the presence of a fibrotic capsule, histologically resembling the outer capsule of chronic subdural hematoma and is thought to grow due to repeated bleeding from the new blood vessels in the capsule2,3.
Imaging:
- CT scan shows a well-defined hypodense lesion with clear borders, surrounding edema and mass effect1.
- On MRI, it appears as hyperintense on T1 and T2 sequences with hypointense rim on T2 sequences.
- Core of the lesion often shows bright signal intensity on DWI due to subacute blood products mimicking an Abscess.
- The wall is uniform in thickness (measuring 1-3mm)2. SWI sequence demonstrates a ring like wall more clearly with low signal intensity2. Coexistence of these signs could distinguish CEIH from brain tumors and brain abscesses1.
- The hematoma envelope (“ring”) is intact in CEIH, but the ring in tumors is often partially or completely missing and is of an uneven thickness1.
- On post contrast study, the enhancement is often variable from mild to no enhancement2.
- Although the outer membrane of the chronic encapsulated intracerebral hematoma is rich in small vessels, the density of the vessels may be much less than in a hypervascular tumor, therefore, the outer membrane of the hematoma does not show hyperperfusion on 3D-ASL1.
Management:
- To prevent recurrence of the hemorrhage originating from the capsule’s thin – walled capillaries, complete excision of the haematoma along with its capsule is mandatory.
- However in our case, only aspiration was done due to diagnostic conspiracy & underlying coagulopathy, following which the aspirated contents were sent to lab which showed degenerative RBCs and no bacterial growth.
Differential diagnosis:
- Cerebral abscess
- Cystic intracerebral tumors
Conclusion:
- In a patient with history of slowly progressive neurological deficits and altered coagulation profile without any fever or raised counts mandates to consider the possibility of CEIH over cerebral abscess.
- On imaging, absent dual rim sign on SWI/T2, low signal on ASL and core T1 hyperintensity favoured CEIH.
| Chronic encapsulated intracerebral haematoma (CEIH) | Cerebral abscess | Cystic intracranial tumours |
| T1 hyperintense | T1 hypointense | T1 hypointense or hyperintense |
| ASL shows hypointense rim | ASL may show bright rim | ASL often shows bright rim |
| Diffusion restriction | Diffusion restriction | Variable diffusion restriction |
| No double rim sign on T2/FLAIR | Double rim sign on T2/FLAIR | No double rim sign on T2/FLAIR |
| Hemosiderin rim on SWI/T2 | May show hemosiderin rim | Glioblastomas may show thick irregular/broken hemosiderin rim |
| May or may not show ring enhancement | Continuous smooth peripheral enhancement | Thick irregular peripheral or central enhancement |
REFERENCES :
- Zhou, B. (n.d.). Imaging Diagnosis of Chronic Encapsulated Intracerebral Hematoma, a Comparison of Computed Tomography (CT) and Magnetic Resonance Imaging (MRI) characteristics Sainan Cai 1
- Kamide, T., Seki, S., Suzuki, K.-I., Aoki, T., Hirano, K.-I., Takahashi, M., & Nomura, M. (2016). A chronic encapsulated intracerebral hematoma mimicking a brain tumor: Findings on arterial spin labeling of MRI. The Neuroradiology Journal, 29(4), 273–276
- Shimizu, K., Sadatomo, T., Hara, T., Ohba, H., Yuki, K., & Kurisu, K. (2017). Frequency and predicting factors on chronic expanding intracerebral hematoma in spontaneous intracerebral hemorrhage. Journal of Stroke and Cerebrovascular Diseases: The Official Journal of National Stroke Association, 26(7), 1541–1546. 4. Marutani, A., Nagata, K., Deguchi, J., Nikaido, Y., & Kazuki, S. (2015). A case of recurrent hemorrhages due to a chronic expanding encapsulated intracranial hematoma. Case Reports in Neurology, 7(3), 173–180.

Add a Comment
You must be logged in to post a comment