October 2025
CASE HISTORY
- A 43-year-old lady presented with chronic headache of 15 years. Headache aggravated on prolonged standing and walking. Headache was initially diagnosed as tension type. It got better after using abdominal binders.
- Patient started developing gait issues since past 5 years and was misdiagnosed as seizure disorder and put on anti-epileptics.
- Patient has memory disturbances since past 2 years.
- Past history of multiple lumbar punctures for CSF analysis and spinal anaesthesia for abdominal surgeries.
CASE CONTRIBUTED BY
Dr. Shilali M S, Department of Radiology, Manipal Hospitals, Kanakapura Road, Bangalore.
Dr. Yashwanth A S, Department of Radiology, Manipal Hospitals, Kanakapura Road, Bangalore.
Dr. Chaitra P Adiga, Department of Radiology, Manipal Hospitals, Kanakapura Road, Bangalore.
Dr. Lakshmikanth G N, Department of Radiology, Manipal Hospitals, Kanakapura Road, Bangalore.
Dr. Sharath Kumar G G, Department of Radiology, Manipal Hospitals, Kanakapura Road, Bangalore.
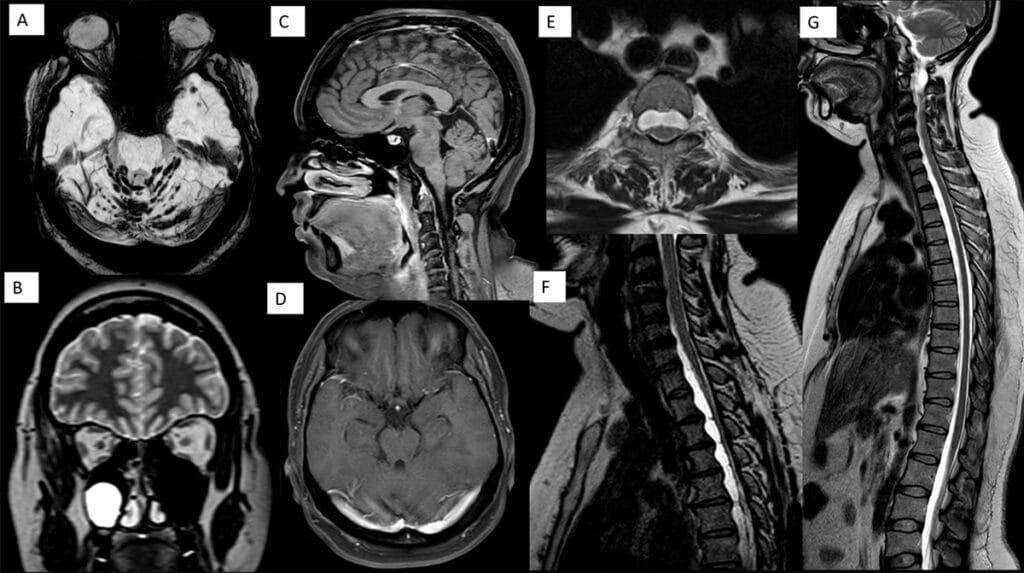
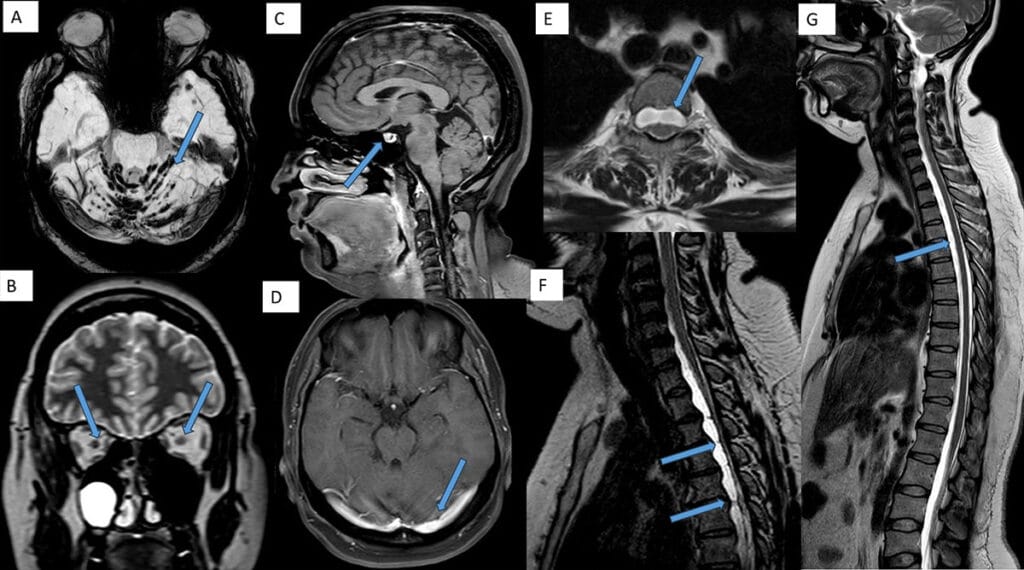
- A – Axial SWI image of brain showing hemosiderin deposits on cerebellar folia and vermis – posterior fossa superficial siderosis(arrow).
- B – T2 weighted coronal image showing collapsed bilateral peri-optic CSF sheaths(arrows).
- C – Sagittal post gadolinium T1 weighted fat saturated image showed mild pituitary congestion(arrow). Distended superior sagittal sinus may also be appreciated in the image. No brain sagging.
- D – Axial post gadolinium T1 weighted fat saturated image showing distended transverse sinuses(arrow). No abnormal meningeal enhancement/subdural collections.
- E , F and G – T2 weighted axial and sagittal images of spine showed ventral spinal longitudinal epidural collection (SLEC) with thin septations within extending from C5 to D11 vertebral levels – chronic/organized SLEC /festooned dura appearance(arrows). No discogenic spurs on screening CT of spine(image not shown).
Diagnosis: Chronic Spontaneous Intracranial Hypotension
Background: Spontaneous intracranial hypotension is a rare secondary headache disorder. It is often misdiagnosed due to its varied clinical presentations and is one of the treatable causes of headache.
Pathology: Majority of SIH is caused by spontaneous CSF leak through dural defects, leaking / ruptured meningeal diverticula or due to CSF-venous fistula (CVF). Most leaks originate in the spine, making spinal imaging crucial.
Clinical presentation: Typical symptom in acute stage is orthostatic headache (worse upright, better lying down). In chronic stage, orthostatic nature of the headache is lost and headache is non-specific in nature. Other symptoms may include nausea, dizziness, tinnitus, double vision, cranial nerve palsies and cognitive issues.
Diagnosis: Neuroimaging, primarily including MRI of brain and spine, screening CT spine and ultra-fast dynamic CT myelography. Imaging features of brain may disappear over time in chronic SIH despite persistence of the leak.
Neuro-imaging features:
MRI Brain Findings (Qualitative):
- Diffuse dural enhancement
- Dural enhancement in IAC
- Dural venous sinus engorgement
- Subdural effusions or hematomas
- Brain sag/Cerebellar tonsillar descent
- Pituitary engorgement
- Suprasellar cistern effacement
- Collapsed peri-optic CSF sheath
MRI Brain Findings (Quantitative):
- Mammillopontine distance < 6.5 mm
- Pontomesencephalic angle < 50˚
- Interpeduncular angle < 40.5˚
MRI Spine Findings:
- Spinal longitudinal epidural collection (SLEC)
- Dural enhancement
- Dilated epidural veins
CT Findings:
- Brain – Layered cake skull appearnce (calvarial hyperostosis)
- Spine – Discogenic spurs
Ultra-fast dynamic CT myelography, digital subtraction myelography, MR myelography maybe utilised to detect the site of CSF leak.
Treatment
- Treatment options for spinal longitudinal epidural collections (SLECs) caused by ventral dural cerebrospinal fluid leaks include epidural blood patching and surgical repair.
- Epidural Blood Patching:
- Targeted Patching: Targets the suspected or confirmed site of the CSF leak. It is more effective for unorganized SLECs, with a resolution rate of 54%.
- Intra-SLEC Patching: Involves direct injection into the organized SLEC. It is more effective for organized SLECs, with a resolution rate of 33%, compared to 4% with traditional targeted patching. However, it requires precise needle placement and may have a higher risk of rebound intracranial hypertension.
- Surgical Repair:
- Recommended for cases where patching fails. Surgery has a high success rate, with 95% of patients achieving SLEC resolution and 83% reporting complete symptom relief.
- Prompt diagnosis and treatment are critical, as organized SLECs are less likely to resolve with patching. Intra-SLEC patching offers a novel approach for organized SLECs, but surgery remains the most definitive treatment.
In this case, exact site of the leak was not identified. Patient was counselled for further imaging evaluation/ultra-fast dynamic CT myelography to locate the exact site of leak and about the treatment options (intra-SLEC patching and surgical repair) for further prevention of superficial siderosis and its consequences. A multidisciplinary meeting involving neurologists and neurosurgeons to discuss the same was also advised.
Due to the chronic nature of the CSF leak, the brain imaging findings were compensated and features of acute spontaneous intracranial hypotension were absent, resulting in low SIH scores (Mayo score and Bern score).
Chronic SIH is an elusive disorder with deceptive presentation and our case demonstrates the importance of evaluation of patients presenting with chronic headache and isolated posterior fossa superficial siderosis to look for spinal CSF leak/evaluate for spontaneous intracranial hypotension. Identifying and addressing surgically correctable cause such as a dural defect is important to prevent disease progression.
References
- Callen, A. L., Timpone, V. M., Schwertner, A., Zander, D., Grassia, F., Lennarson, P., Seinfeld, J., Lillehei, K. O., Birlea, M., & Thaker, A. A. (2022). Algorithmic multimodality approach to diagnosis and treatment of spinal CSF leak and venous fistula in patients with spontaneous intracranial hypotension. American Journal of Roentgenology, 219(2), 292–301. https://doi.org/10.2214/AJR.22.27485
- Callen AL, Pisani Petrucci SL, Lennarson P, Sedrak MF, Gutierrez A, Mamlouk MD. Efficacy of Traditional Epidural Patching versus Patching within Spinal Longitudinal Extradural Collections for Ventral Dural Cerebrospinal Fluid Leaks. Radiology. 2025;314(3):e242194. doi:10.1148/radiol.242194

Add a Comment
You must be logged in to post a comment