Oct 2022
CASE HISTORY:
•A 21 year old male was brought for evaluation of fever since 45 days associated with holocranial headache for 30 days and altered sensorium for 20 days .
Working clinical diagnosis of chronic meningoencephalitis was made for which cross sectional imaging was requested.
Case contributed by –
Dr Ankit Arora, Senior Resident
Department of Neuroimaging and Interventional Radiology, NIMHANS Bangalore
Dr Sabha Ahmed, Senior Resident
Department of Neuroimaging and Interventional Radiology, NIMHANS Bangalore
Dr Jitender Saini, Professor
Department of Neuroimaging and Interventional Radiology, NIMHANS Bangalore
FINAL DIAGNOSIS
Neuromelioidosis
●Neuromelioidosis is caused by Burkholderia pseudomallei , a non spore forming gram negative aerobic bacillus found in soil and water in tropical nations.(1,2)
●Inhalation, via skin abrasions and ingestion account for the various means of entry into the human body, thereby inflicting the lungs, skin and genitourinary system. (1)
●Central nervous system infliction is rather uncommon and has sinister clinical manifestations of meningitis, abscesses, cranial neuritis and meningoencephalitis.
Imaging findings :
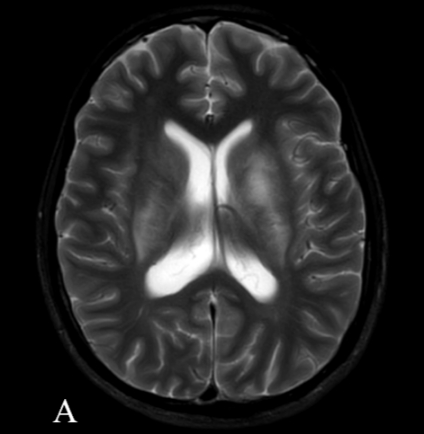
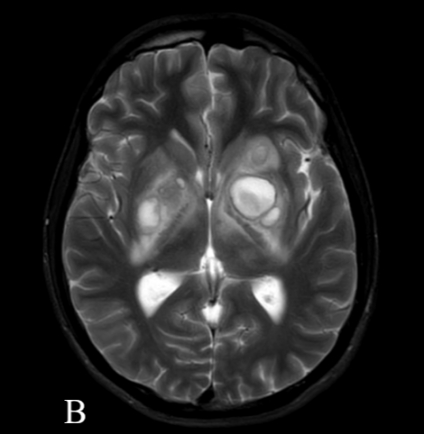
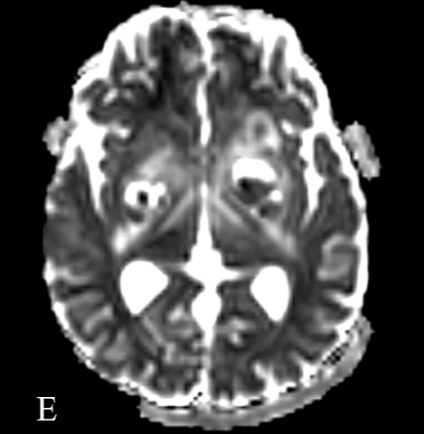
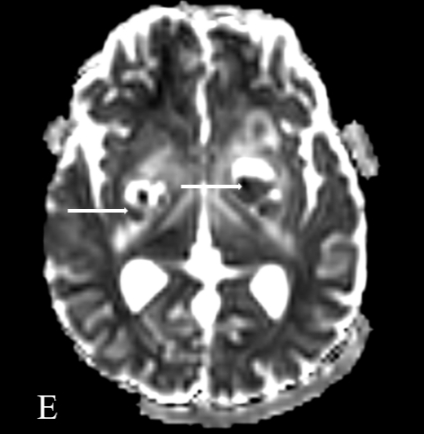
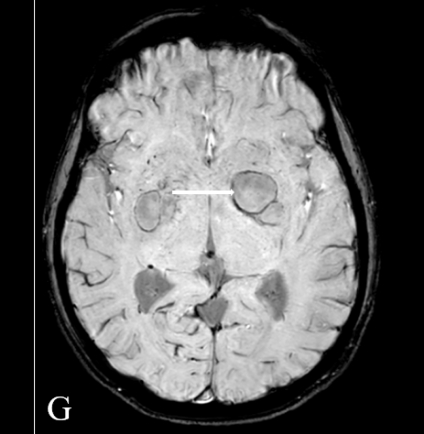
1.Commonly encountered phenotype of CNS infection include rounded or oval/ tubular rim enhancing cerebral microabscesses.
2.Distinct propensity of involvement and extension along white matter tracts , with involvement of commissural and projection fibers and thereby spread to the contralateral hemisphere.
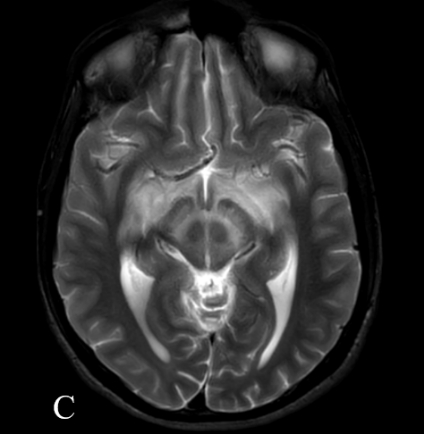
3.Relatively frequently encountered imaging phenotype is that of brainstem and cranial nerve involvement in particular cranial nerve V.
4.A rather distinguishing feature in CNS melioidosis is the diffusely extensive involvement of cranial nerves and contiguous intraaxial spread into the brain stem, with resultant trespassing microabscesses.
5.B. pseudomallei can also gain direct entry into the CNS via direct extension of scalp or skull infection with scalp osteolytic lesions serving as harbinger of pathogen entry.
6.Lastly, spinal cord abscesses and epidural collections may also be encountered.
●CNS melioidosis is associated with high mortality and morbidity.
●The most appropriate antibiotic treatment for melioidosis is still being debated.
●Chadwick et al (3) recommended the administration of intravenous ceftazidime or imipenem for the eradication phase followed by oral maintenance therapy with either trimethoprim/sulfamethoxazole or doxycycline for six to eight months. Kandasamy et al (4) proposed the administration of ceftazidime or meropenem alone or with the addition of co-trimoxazole as the most active regime.
REFERENCES
1.Mannam P, Arvind VH, Koshy M, Varghese GM, Alexander M, Elizabeth SM. Neuromelioidosis: A Single-Center Experience with Emphasis on Imaging. Indian Journal of Radiology and Imaging. 2021 Jan;31(01):057-64.
2. Hsu CC, Singh D, Kwan G, Deuble M, Aquilina C, Korah I, Norton R. Neuromelioidosis: Craniospinal MRI Findings in Burkholderia pseudomallei Infection. J Neuroimaging. 2016 Jan-Feb;26(1):75-82.
3.Chadwick DR, Ang B, Sitoh YY, et al. Cerebral melioidosis in Singapore: a review of five cases. Trans R Soc Trop Med Hyg 2002;96:72-6.
4.Kandasamy Y, Norton R. Paediatric melioidosis in North Queensland, Australia. J Paediatr Child Health 2008;44:706-8.















Neuro meliodosis
Cerebral toxoplasmosis
Multiple thin smooth ring enhancing lesions with central restriction in bilateral capsuloganglionic regions with perilesional edema and pachymeningeal enhancement in the left frontal and temporal regions
DD: pyogenic abscess with meningitis
Fungal etiology – cryptococcomas with meningitis ( immunocompromised state to be ruled out)
Neuromeliodosis
Acute necrotising encephalitis