June 2021
••A 29 year old male presented with first episode of left focal seizures.
Case contributed by –
Dept of Neuroimaging and Interventional Neuroradiology, AIIMS, New Delhi
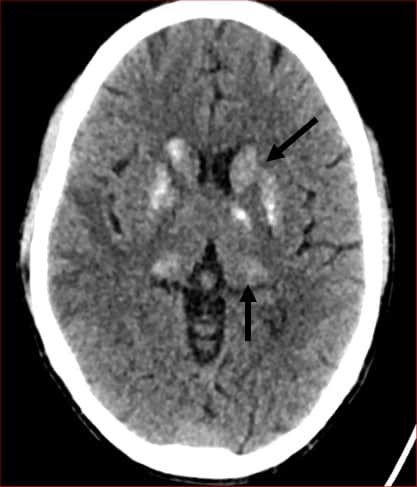
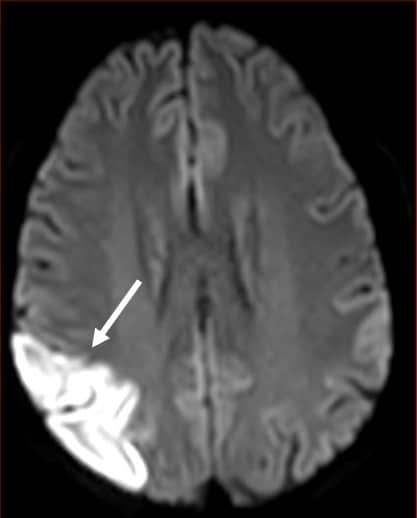
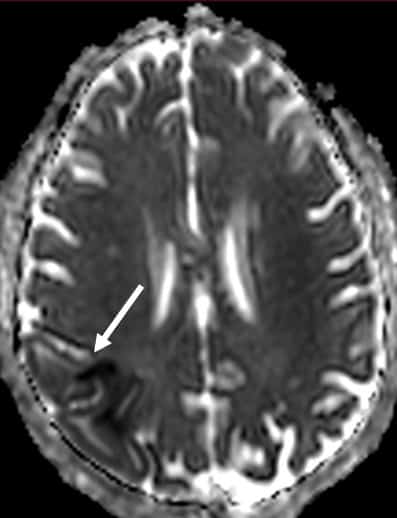
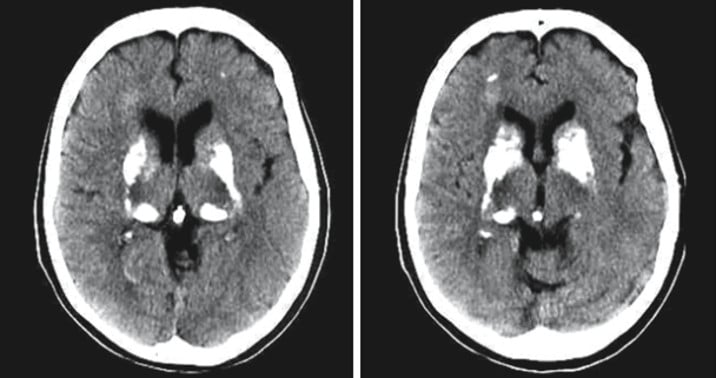
Axial NCCT image of the brain shows calcifications involving bilateral basal ganglia and thalami. Axial T1 and T2-w images show hyperintense basal ganglia and thalami, with corresponding areas showing blooming in axial SWI, consistent with calcifications (black arrows). Right parietal lobe shows a focal area of hyperintense signal involving both grey and white matter in axial T2-w image, which shows hyperintense and hypointense signals in DWI and ADC map respectively, suggestive of diffusion restriction and consistent with acute infarct (white arrows).
Final Diagnosis: FABRY’S DISEASE
- Pointers helping to arrive at a differential diagnosis in this case are:
- Young
- Male
- First presentation is seizure (indicating that basal ganglia / thalami classifications are largely asymptomatic)
- Symmetric basal ganglia and thalami (pulvinar) classifications
- Ischemic infarct
- Three differential diagnosis that includes most of the pointers listed above are
- Fabry’s disease
- Mitochondrial myopathies with prototype being MELAS
- SLE with intracranial manifestations (CNS lupus)
- Fabry’s disease
- Fabry’s disease is a lysosomal storage disorder, due to mutation coding for hydrolase α-galactosidase A. Since the disease is transmitted as X linked recessive disorder, it is expressed in its classical form in males. Females are usually heterozygous for the disease (One normal X, and one mutated X chromosome) and present with variable severity. (1)
- T1 pulvinar hyperintensity and calcifications are specific findings (which are usually asymptomatic) and usually present with acute ischemic strokes. Dolichoectasia of vertebrobasilar system is also a commonly associated finding.
- MELAS and other mitochondrial myopathies
- MELAS may present with basal ganglia calcifications and infarct, and present with seizures. However it would not be the first presentation. Usually they present with infarcts in parieto-occipital lobes not limited to vascular territory in the first presentation, and only in older patients basal ganglia / thalamus calcifications are usually seen (presumably due to multiple infarcts over time and secondary dystrophic calcifications)
- MERRF usually have no stroke or stroke like episodes, but when present considered as MERRF/MELAS overlap.
- CNS lupus
- CNS manifestations of SLE are variable. Dense symmetric calcifications of basal ganglia & thalami, and infarcts are both reported (2), and they can co-exist in 7.4% of patients. Raymond et al also noted that calcifications did not correlate with severity of the disease (hence may be asymptomatic).
Although this pattern of (asymptomatic and symmetric) calcifications is seen in metabolic disorders including hyperparathyroidism, hypoparathyroidism, Fahr’s disease (including SLC20A2, XPR1, PDGFB, PDGFRB mutations), infarcts are uncommon thus ruling out these disorders.
Mineralizing microangiopathy may present with basal ganglia calcifications and infarcts. However, the calcifications are usually not dense (as in our case), calcifications spare thalamus, and infarcts are limited to basal ganglia, as the main pathology is usually limited to lenticulostriate arteries. (3)
References
- Olivier Lidove et al. Imaging Features of Fabry Disease. American Journal of Roentgenology. 2006;186: 1184-1191. 10.2214/AJR.05.0019
- Raymond AA, Zariah AA, Samad SA, Chin CN, Kong NC. Brain calcification in patients with cerebral lupus. Lupus. 1996 Apr;5(2):123-8. doi: 10.1177/096120339600500207. PMID: 8743125.
- Shanley DJ. Mineralizing microangiopathy: CT and MRI. Neuroradiology. 1995;37 (4): 331-3.
- Magnetic Resonance of Myelination and Myelin Disorders, M.S.van der Knaap,J.Valk, 3rd edition, Springer.
- Symmetrical and bilateral basal ganglia calcification. Case series and literature review. October 2018G. aceta medica de Mexico 154(2) DOI: 10.24875/GMM.M18000137











Fabrys disease
Fabrys disease
Hypoparathyroidism
SLC20A2 mutation
CJD
CJD
MERRF
MELAS