January 2022
CASE HISTORY
17-year-old female presenting with •Acute onset of right upper and lower limb weakness •Giddiness, Deviation of mouth and slurring of speech
Clinical Diagnosis: • Young stroke (6 hours 40 minutes from onset to imaging)
Investigation ordered – MRI Brain with MRA (Follow up images are provided for comparison)
Case contributed by –
Institute affiliation: KMCH, Coimbatore
Authors – Dr. Meena Nedunchelian (PG resident during case)
Dr. Nikhil HA (IR fellow)
Dr. Senthil Kumar E (Consultant Neurologist)
Dr. Shriram Varadharajan (Consultant Neuroradiologist)
 |  |  |  |
 | 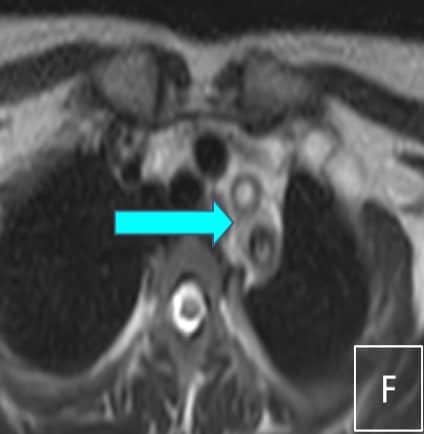 |  |  |
Figure Captions:
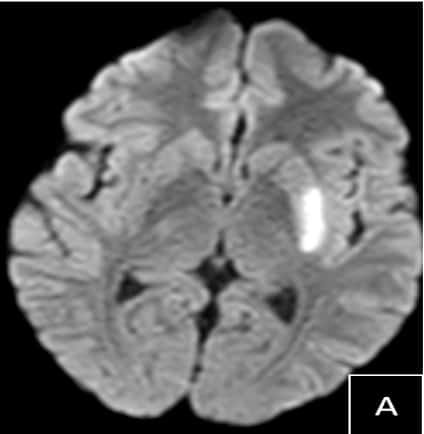
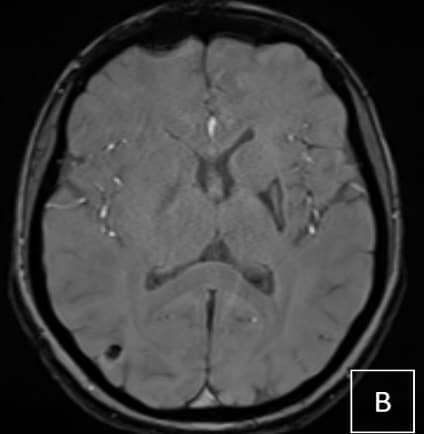
A. DWI axial shows restricted diffusion in left posterior putamen, suggestive of acute infarct
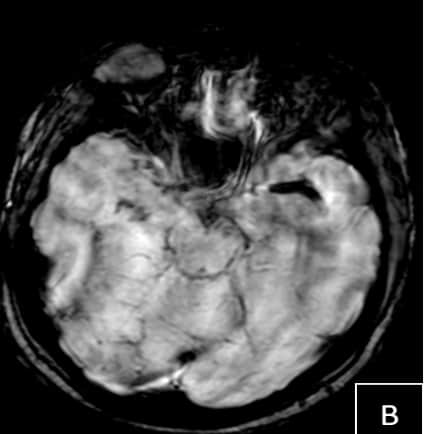
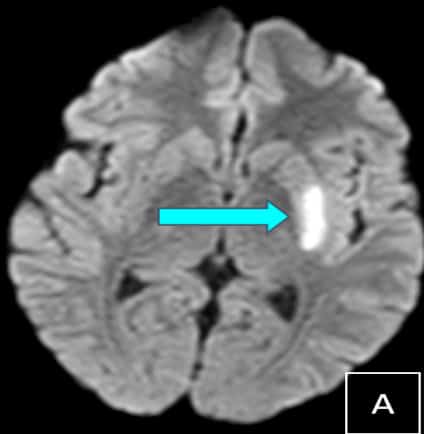
B.SWI axial shows long segment blooming (susceptibility vessel sign) involving left M1 segment of the MCA.
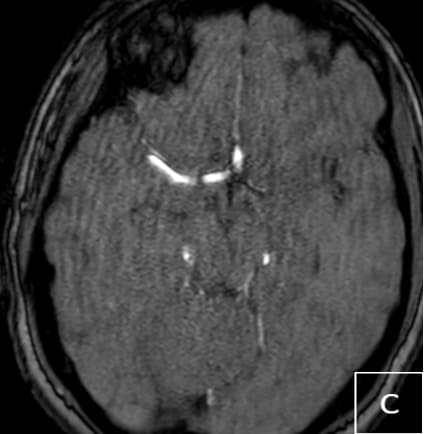
C. TOF MRA brain shows corresponding loss of flow signal along the left MCA
D. TOF MRA neck shows non visualization of the left subclavian, common carotid, internal and external carotid and left vertebral arteries
E. Axial source images of TOF MRA Neck shows thickening of the distal aortic arch
F. Axial T2 images of thorax show loss of flow void and wall thickening in left common carotid and subclavian arteries
G. AXial CTA re-demonstrates wall thickening along the distal aortic arch. H. Sagittal MIP of CT Angiogram also shows thickening along mid and distal thoracic aorta
Follow up images
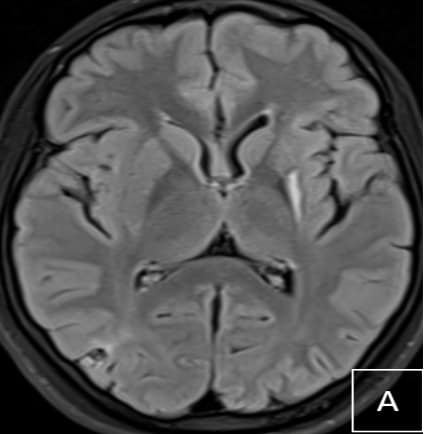
A FLAIR Axial shows chronic infarct in the left posterior putamen
B SWI axial shows peripheral hemosiderin staining s/o hemorrhagic gliosis
C TOF MRA shows interval recanalization of left MCA
C CT angiogram shows interval decrease in the wall thickening involving distal arch of aorta.
Final Diagnosis & Clinical outcomes :
Final diagnosis – Aortoarteritis with left MCA thrombo-embolic occlusion
ACR criteria for Takayasu arteritis (TA) was positive and her score was 5/6 (Type IIB TA)
Differential diagnosis of young stroke – Inflammatory/Non inflammatory arteriopathies, Cardiac/ Embolic causes, Hematological- Hypercoagulable states, Genetic, Trauma-Dissection
Treatment & Clinical outcome
Pulsed methylprednisolone for five days, antiplatelet, atorvastatin and other supportive care
Physio and occupational therapy
Able to walk independently and was discharged in stable condition
Learning Points – Clinical
•Consider vasculitis as differential in young patients with stroke
•Takayasu arteritis (TA) is commonly seen in the second and third decade females
•Proximal arch vessels involvement with distal extension can act as source of embolic LVO
•ACR Classification Criteria or the EULAR/PRINTO/PRES criteria for c-TA are used
•These criteria include the addition of hypertension, non-inflammatory conditions such as fibromuscular dysplasia, pulse deficit, claudication and increased acute phase reactants
•Pharmacological therapy is the mainstay of TA and Glucocorticoids are the most effective agent for patients with active TA
•Mechanical thrombectomy may be considered for eligible patients with large vessel occlusion stroke secondary to TA based on clot burden and medical futility
•Our patient had favorable clinical outcome with medical and supportive management with follow up imaging showing MCA recanalization as well as reduced arch vasculitis
Learning Points – Imaging
•Computed tomography and magnetic resonance imaging besides conventional angiography as imaging techniques have been incorporated for imaging diagnosis
•Although CT with CTA is commonly used worldwide for detection of LVO, MRI with MRA is often used for the etiological workup of stroke in the young patients
•Stroke imaging should always include evaluation of arch and neck vessels
•Multifocal narrowing on MRA with mixed parenchymal changes (ischemic and hemorrhagic infarcts, microbleeds) can be seen in vasculitis
•Isolated eccentric or circumferential wall thickening involving multiple vessels with parenchymal changes can also be predictive of vasculitis
•Flow related changes on non contrast MRA needs CTA confirmation
•MRI (contrast vessel wall) allows for assessment of wall and lumen
•Vessel wall enhancement on CT/MRI indicates active disease and can guide steroid initiation while follow up imaging can be used to monitor treatment response
Thank you & References
1.Giuseppe Lanni, Alessia Catalucci, Laura Conti, Alessandra Di Sibio, Amalia Paonessa, Massimo Gallucci, “Pediatric Stroke: Clinical Findings and Radiological Approach”, Stroke Research and Treatment, vol. 2011, Article ID 172168, 11 pages, 2011. https://doi.org/10.4061/2011/172168
2.Gao P, Dmytriw AA, Wang T, et al. Contemporary Challenges of Acute Ischemic Stroke in Takayasu Arteritis. Stroke. 2020;51(10):e280-e284. doi:10.1161/STROKEAHA.120.030249
3.Sikaroodi H, Motamedi M, Kahnooji H, Gholamrezanezhad A, Yousefi N. Stroke as the first manifestation of Takayasu arteritis. Acta Neurol Belg. 2007;107(1):18-21.
4.Dejaco C, Ramiro S, Duftner C, et al. EULAR recommendations for the use of imaging in large vessel vasculitis in clinical practice. Annals of the Rheumatic Diseases 2018;77:636-643.
5.Hellmich B, Agueda A, Monti S, et al,2018 Update of the EULAR recommendations for the management of large vessel vasculitis,Annals of the Rheumatic Diseases 2020;79:19-30.