March 2021
A 22-year-old male presented with complain of headache, vomiting for 4 to 6 weeks. Associated with weakness of all limbs and loss of bladder/bowel control for 10 days.
Case contributed by –
Department of Diagnostic and Intervention Radiology, AIIMS, Jodhpur.
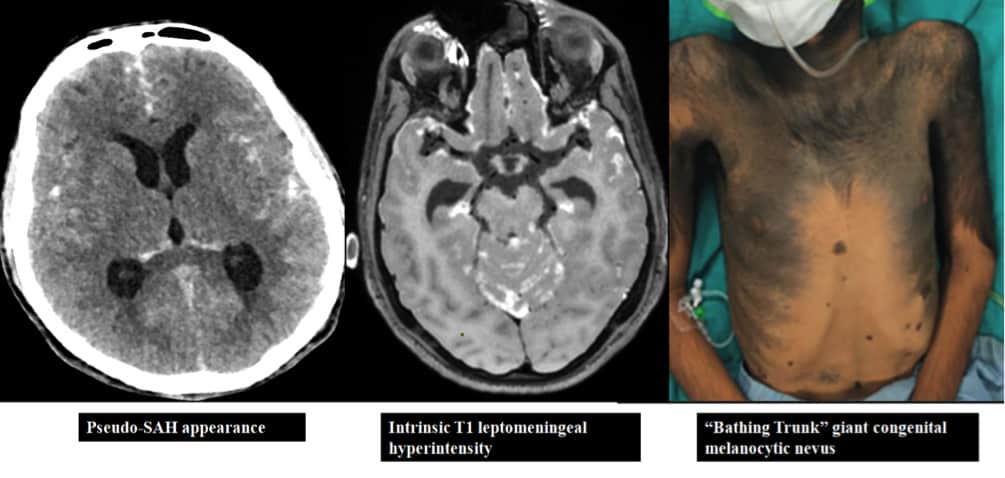
Figure 1:The non-contrast CT head axial (a & b) & sagittal (c) images shows diffuse and nodular sulcal hyperattenuation with mild hydrocephalus.
Note the nodular lesion along right frontal convexity (black arrow), irregular hyperattenuating leptomeningeal thickening along the brainstem surface (dashed black arrowhead) and superior cerebellar cistern (white arrow).
The volume rendered TOF MRA image (d) and CT angiogram (not shown) did not show any aneurysm or vascular malformation.
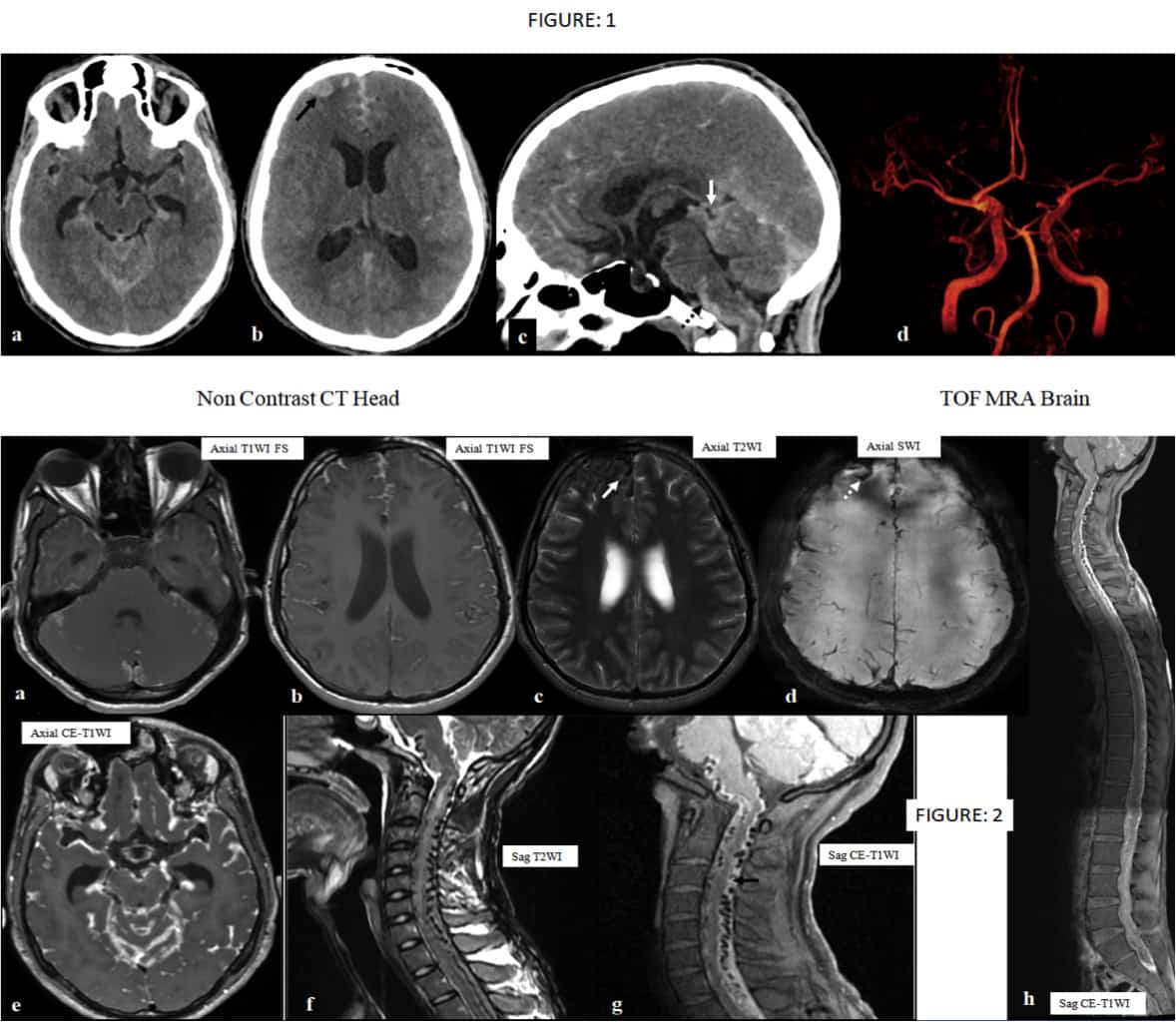
Figure 2:The axial fat-saturated T1 images (a & b) diffuse nodular leptomeningeal hyperintensity with dural sparing. The thickened leptomeninges showed hypointense signal on the T2 image (c) and blooms on the susceptibility weighted image (d). The post contrast T1 image (e) showed irregular and nodular enhancement. The sagittal T2 (f) and T1FS (g) cervical spine showed multiple flow voids along the surface of the cord with intrinsic cervical cord hyperintensity (due to leptomeningeal infiltrates along vessels leading to secondary venous hypertension). Note the leptomeningeal hyperintensity on the T1 images (black arrow).
Whole spine T1 post contrast fused sagittal image (h).
Final Diagnosis: Neurocutaneous Melanomatosis
- Neurocutaneous melanosis is a rare congenital phakomatosis characterized by large or multiple congenital melanocytic nevi and benign or malignant pigment cell tumors of the leptomeninges. Potential for malignant degeneration has a prevalence of 40–60% according to different reports. (1),
- Leptomeningeal Melanosis can mimic subarachnoid hemorrhage on imaging.
- Upto 12% of individuals with giant congenital nevi develop symptomatic neurocutaneous melanosis. (2)
- The leptomeningeal process in neurocutaneous melanosis involves the parenchyma, choroid plexus, and ventricular ependyma with sparing of the duramater.
- The primary differential diagnosis for NCM is metastatic melanoma arising either in the central nervous system or the skin as a primary site. (3)
References:
- Chu WC, Lee V, Chan YL, Shing MM, Chik KW, Li CK, Ma KC. Neurocutaneous melanomatosis with a rapidly deteriorating course. American journal of neuroradiology. 2003 Feb 1;24(2):287-90.
- Ramaswamy V, Delaney H, Haque S, Marghoob A, Khakoo Y. Spectrum of central nervous system abnormalities in neurocutaneous melanocytosis. Developmental Medicine & Child Neurology. 2012 Jun;54(6):563-8.
- Demir MK, Aker FV, Akinci O, Ozgultekin A. Case 134: primary leptomeningeal melanomatosis. Radiology. 2008 Jun;247(3):905-9.

spinal dural arteriovenous fistula causing intracranial subarachnoid hemorrhage:
Other thoughts:
Melanosis
Vascular malformation with venous congestion
Diffuse extensive intracranial and spinal leptemeningeal exhudates and enhancement – CNS tuberculosis / Leptemeningeal carcinomatosis.
May be glioneuronal tumor
But those flow voids are odd
Diffuse leptomeningeal melanomatosis
Diffuse leptomeningeal glioneuronal tumour
Leptomeningeal carcinomatosis
Tubercular meningitis
Type 5 DAVF
Diffuse leptomeningeal glioneural Tumor