August 2025
CASE HISTORY
- A 29-year-old man complains of neck pain extending to left side of shoulder and diffuse back pain for 5 years.
- Symptoms aggravate on driving, prolonged standing, lifting loads.
- No radiating pain/ weakness/ numbness.
- No history of fever or weight loss.
- TB GENE XPERT- Negative, Hb- 17.4g, PCV- 52.8, ESR and CRP -Normal, WBC Count-7760
CASE CONTRIBUTED BY
Dr. Nithish G, Department of Radiology, Manipal Hospitals, Kanakapura Road, Bangalore.
Dr. Veekshit Shetty, Consultant Neurosurgery, Manipal Hospitals, Kanakapura Road, Bangalore.
Dr. Dayanand Linge Gowda, Department of Radiology, Manipal Hospitals, Kanakapura Road, Bangalore.
Dr. Vidya. M. N., Lead Consultant Pathologist, Manipal hospitals, Old airport Road, Bangalore.
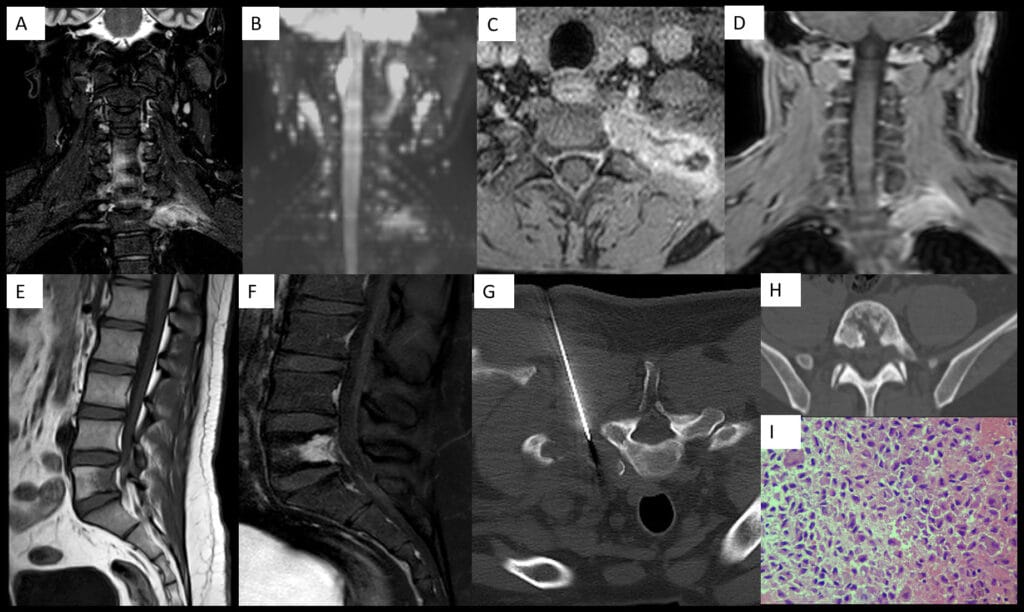
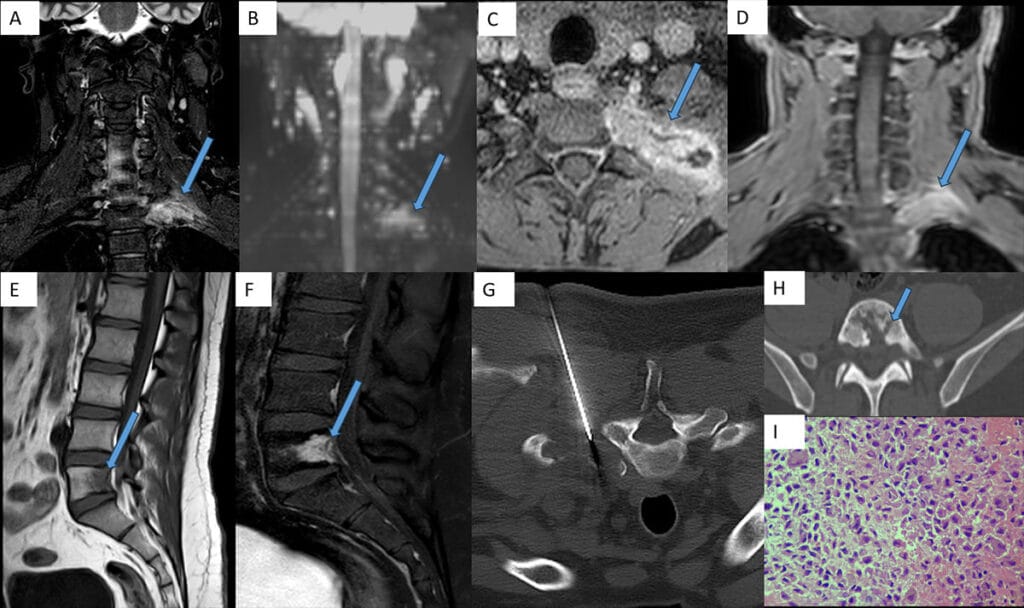
- A – Coronal STIR shows hyperintensity within the left transverse process of T1 vertebra and the posterior aspect of the left 1st rib with soft tissue extension.
- B – Coronal DWI showing diffusion restriction in corresponding areas.
- C and D – Postcontrast axial and coronal T1FS shows expansile lytic lesion with heterogenous enhancement, cortical erosion and soft tissue extension.•E – Sagittal T1 showing hypointenisty within posterior body of L5 vertebra.
- F – Postcontrast sagittal T1FS showing significant heterogenous enhancement of L5 vertebral body.
- G- Prone CT-guided biopsy of expansile lytic lesion in left 1st rib through a posterolateral approach
- H – Axial CT showing moth-eaten bone destruction in L5 vertebral body.
- I –Histology reveals sheets of large histiocyte-like cells resembling Langerhans cells, characterised by vesicular nuclei with nuclear grooves. Occasional multinucleated cells are present. The background is rich in eosinophils, with intermixed reactive lymphoid aggregates, plasma cells, and a few neutrophils
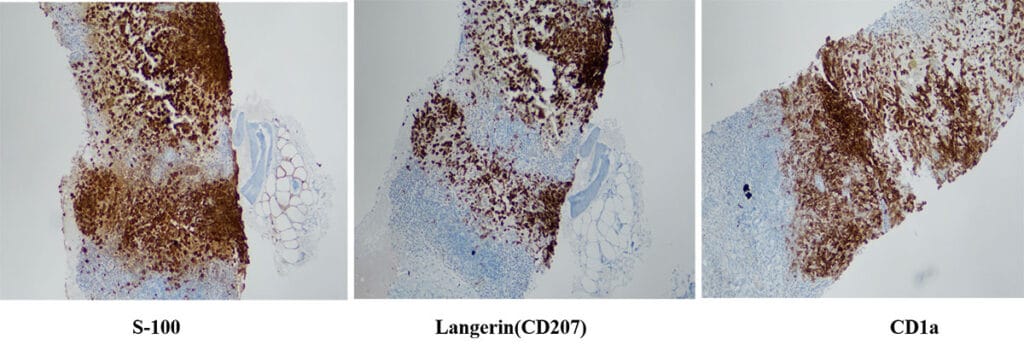
IHC (Immunohistochemistry) positive for S-100, CD207(Langerin) and CD1a antigens
Diagnosis: Langerhans cell histiocytosis(LCH)
Background: Histiocytic disorders are divided into 3 groups: Dendritic cell disorders, Macrophage-related disorders, and Malignant histiocytic disorders. LCH is the most common dendritic cell disorder. Other less common diseases include Erdheim-Chester disease and juvenile xanthogranuloma
Pathology: LCH is a clonal proliferation of cells that resemble Langerhans cells, which are normally present in skin. LCH cells exhibit CD1a, S100, and CD207 antigens and unique intracytoplasmic organelles called Birbeck granules. LCH is divided into 3 groups:
- Unifocal/localised form – 70% – Limited to single /few bones and may involve the lung, and patients present between 5 -15 years of age
- Multifocal unisystem / chronic recurring form – 20% – Involves multiple bones and the reticuloendothelial system, and is accompanied by diabetes insipidus. Patients present between 1-5 years of age
- Multifocal multisystem/fulminant form -10% – fatal. It is diagnosed in first 2 years of life. Characterised by disseminated involvement of the reticuloendothelial system, anemia, and thrombocytopenia
Imaging features :
- Skull –“Punched-out” lytic lesion with bevelled edge and geographic skull. Button sequestrum.
- Spine – Vertebral body is commonly affected. Early lesions appear lytic. MRI shows T1 hypointense, T2 hyperintensity, with areas of enhancement. Vertebra plana occurs later.
- Long bones – Common in children, involve the diaphysis/metaphysis.
Early lesions – lytic, expansile, and aggressive. Less aggressive lesions have cortical thickening and a smooth periosteal reaction. Mature lesions have a sharply defined sclerotic margin - Flat bones – “Floating teeth” if enough alveolar destruction; Lytic lesion with sclerotic rim and surrounding sclerosis in the iliac bone
- Liver – Hepatomegaly, solid or cyst-like lesions and sclerosing cholangitis.
- Lymph nodes -Most common in the neck
- CNS –Diabetes insipidus and neurodegeneration, absent posterior pituitary bright spot, thickening of pituitary stalk
- Lung – Centrilobular nodules or cysts of varying sizes, with mid- to upper-lung distribution and sparing of costophrenic angles. Common in adults with smoking.
Treatment
- Skull/single long bone – Curettage with intralesional steroid injection or radiation therapy. Multiple bone -Chemotherapy and oral systemic steroids
- Spine – Radiation therapy for lesions at risk of collapse. Spinal fusion or bracing with neurologic symptoms
- Liver/spleen – Chemotherapy and steroids
- CNS – Chemotherapy +/- steroids for active disease with diabetes insipidus.
Retinoic acid and IVIG for neurodegenerative symptoms - Lung – Smoking cessation. Chemotherapy and steroids for persistent/ progressive cases
Differential diagnosis
- Metastasis
- Atypical Tuberculosis – in endemic areas
In our case, isolated spine and rib involvement was seen with absence of other classic regions of LCH involvement like skull, long bones, CNS, lung and reticuloendothelial system.
This case highlights the importance of including histiocytic disorders in the differential diagnosis of aggressive-looking skeletal lesions in young patients and children.
References
- More than Just Langerhans Cell Histiocytosis: A Radiologic Review of Histiocytic Disorders. Jatin Zaveri, Quan La, Gail Yarmish, and Jeremy Neuman.Radiographics 2014 34:7, 2008-2024.
- Shanmugam V, Pozdnyakova O. Langerhans cell histiocytic neoplasms. Pathology Outlines.com website. https://www.pathologyoutlines.com/topic/lymphnodeslch.html. Accessed June 27th, 2025
