June 2025
CASE HISTORY
20 year old male patient presented with headache for 2 days, altered sensorium and single episode of seizure. He had a major road traffic accident one week back.
CASE CONTRIBUTED BY
Dr. Charu Paruthi1, Dr. Reeta Kanaujiya1
1Professor
Department of Radiodiagnosis and IR, VMMC and Safdarjung Hospital, New Delhi
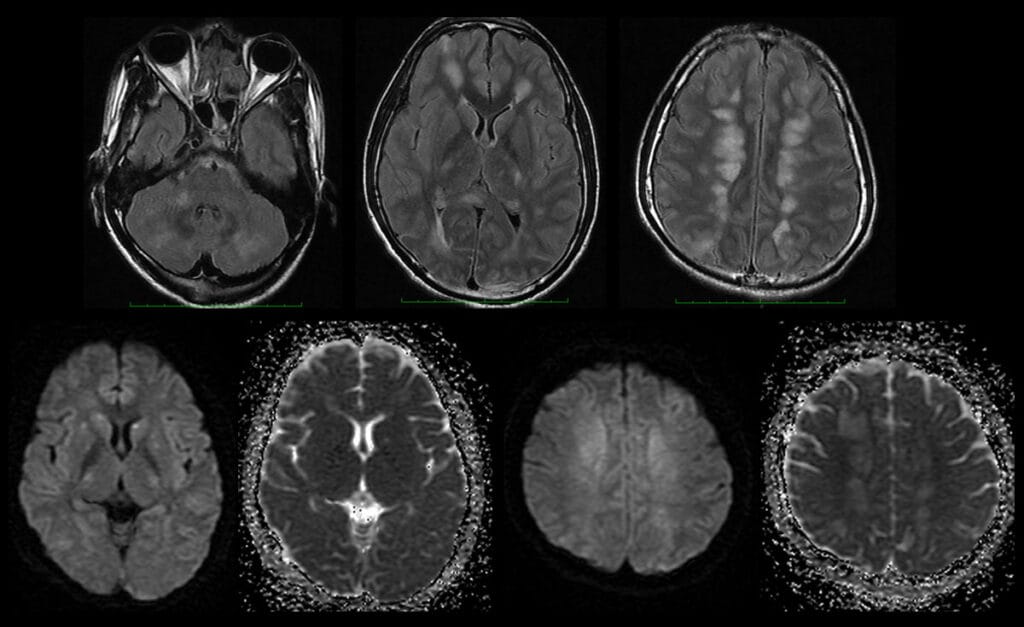
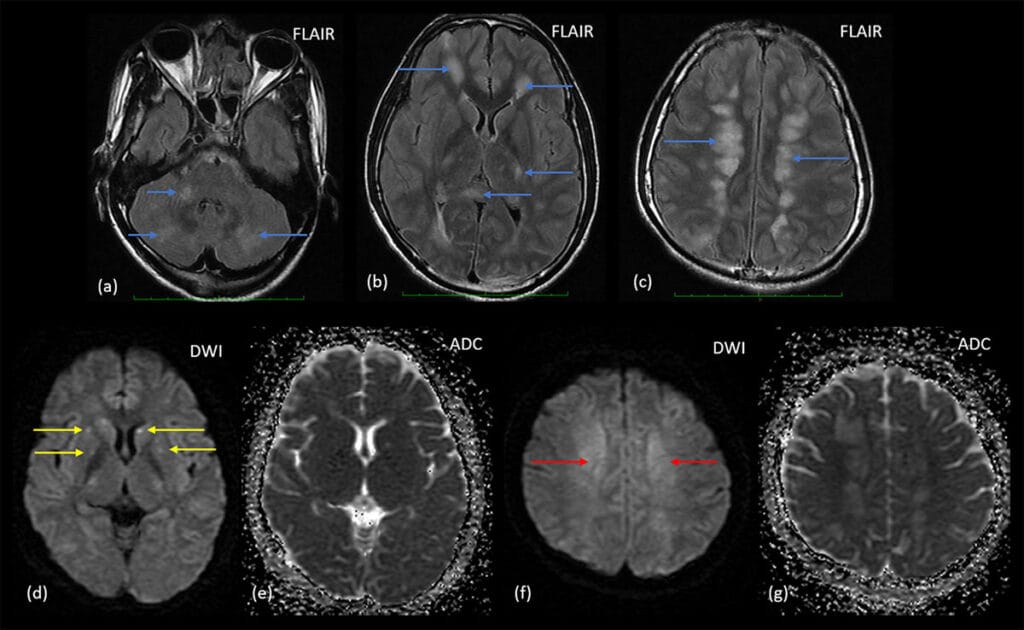
(a-c) FLAIR images show multiple small ill-defined confluent white matter hyperintensities involving bilateral frontal periventricular regions and bilateral centrum semiovale (internal watershed areas), bilateral cerebellar white matter. Roght middle cerebellar peduncle, posterior limb of internal capsule, thalami and splenium of corpus callosum. (d-g) Small punctate areas of diffusion restriction are seen in bilateral basal ganglia. Patchy diffusion restriction is seen in bilateral centrum semiovale.
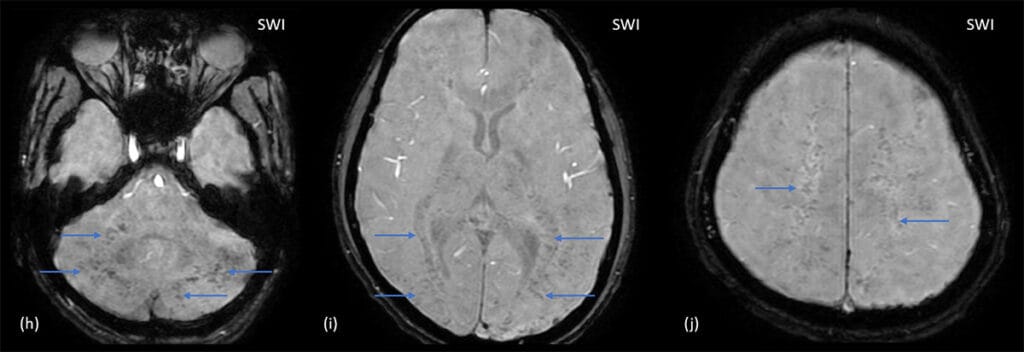
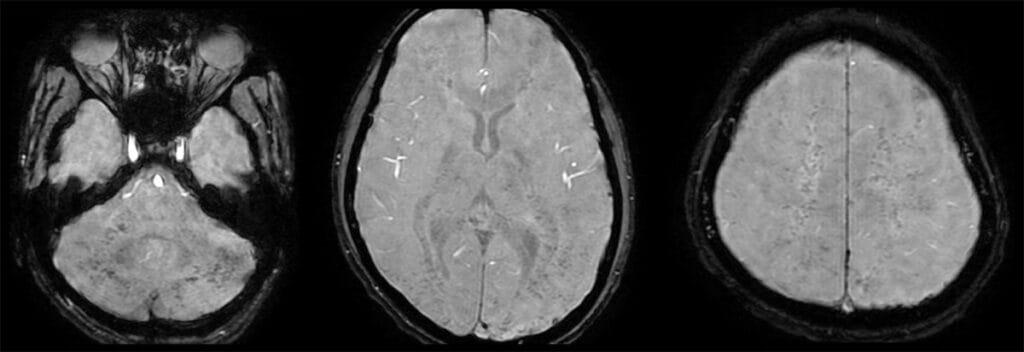
(h-j) SWI images (magnitude) show multile microbleeds diffusely scattered in the involved regions (cerebellar white matter, middle cerebellar peduncles, periventricular white matter and centrum semiovale): WALNUT KERNEL PATTERN. These are more in the central white matter than at gray-white matter junction.

X-ray pelvis with both legs shows fracture of the neck of femur on the right side.
Diagnosis: Cerebral Fat Microembolism
- Cerebral Fat embolism usually occurs secondary to fracture of long bone and may be: Macroembolism (similar to large vessel stroke) or microembolism (concurrent with fat embolism syndrome)
- Cerebral fat microembolism occurs in 1-3% of all fractures and should be suspected in patients with large fractures of long bones, especially lower limb bones, presenting with altered mental status and headaches.
- SWI and DWI are the most useful sequences
- MRI imaging appearance in cerebral microembolism has been classified in three patterns depending upon the stage:
Type 1: Scattered Cytotoxic Edema/starfield pattern
- Most Common
- Reversible, nonspeciific in all embolic events
- Seen in watershed zones, basal ganglia
Type 2: Confluent Cytotoxic /vasogenic Edema in White Matter with petechiae heamorrhages; Walnut Kernel Pattern (SWI)
- Subacute stage (5-14 days after fracture)
- Scattered foci of T2 and diffusion abnormality become more confluent
- On SWI, multiple scattered microhaemorrhages are seen in both the the deep and subcortical white matter (Walnut Kernel Pattern)
Type 3: Type 3: Chronic Sequelae (>14 days)
- Sequelae of infarction, cavitation, scar formation, gliosis, or chronic demyelination
Differentials:
- Diffuse Axonal Injury (DAI): In the setting of trauma, this is a close differential. Microhaemorrhages usually involve only the gray-white matter junction, with relative sparing of deep white matter
- Disseminated Intravascular Coagulopathy
- Septic Emboli
References:
- Kuo KH, Pan YJ, Lai YJ, Cheung WK, Chang FC, Jarosz J. Dynamic MR imaging patterns of cerebral fat embolism: a systematic review with illustrative cases. AJNR. 2014 Jun;35(6):1052-7. doi: 10.3174/ajnr.A3605.
- Giyab O, Balogh B, Bogner P, Gergely O, Tóth A. Microbleeds show a characteristic distribution in cerebral fat embolism. Insights Imaging. 2021 Mar 31;12(1):42. doi: 10.1186/s13244-021-00988-6.
- Sethi D, Kajal S, Saxena A. Neuroimaging findings in a case of cerebral fat embolism syndrome with delayed recovery. Indian J Crit Care Med. 2015 Nov;19(11):674-7. doi: 10.4103/0972-5229.169350.
